Asthma
and COPD are both chronic inflammatory diseases of
the respiratory system, although
characterised by distinct pathophysiological and
clinical features. The inflammatory process in COPD
differs from that
in asthma for inflammatory cells, mediators, inflammatory effects and, consequently,
for response to therapy.
Understanding the main distinct characteristics
of inflammation in asthma and COPD is crucial to comprehend why the two diseases
responses to inhaled corticosteroids (ICSs) and inhaled long-acting β2-agonists
(LABAs) are so different.
Asthma is mainly characterised by airway inflammation,
remodelling and smooth
muscle dysfunction. Acute and chronic airway inflammation
in asthma is due to the recruitment and activation
of a wide
range of inflammatory cells, such as eosinophils, CD4+ T
lymphocytes and mast cells, and to the release of
multiple
mediators (mainly cytokines, interleukin (IL)-4
and 13, and chemokines),
which sustain the inflammatory process.
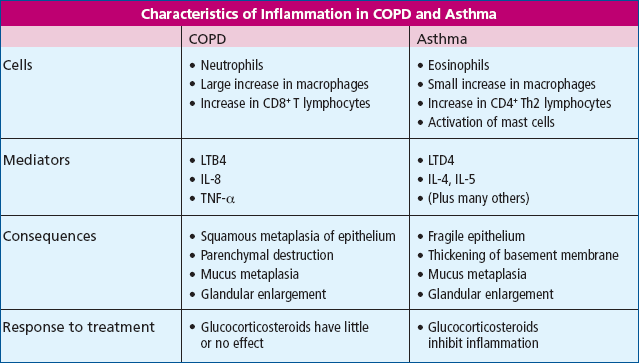
Also COPD is characterised by an inflammatory component,
besides structural
changes and mucociliary dysfunction. However, inflammation
in COPD is associated to an increase in different
inflammatory
cells (CD8+ T lymphocytes, monocytes/macrophages and neutrophils)
and mediators (i.e. IL-8, tumor necrosis factor
(TNF)-α, leukotriene B4) (Fig.
1).1
Figure 1: Characteristics of inflammation in COPD and asthma (GINA guidelines).2
The standard therapy for both the diseases includes the administration of LABAs and ICSs, following a specific therapeutic
strategy and applying a progressive increase in therapy, which are distinctive
for each disease.
In asthma,
ICSs are the first-line therapy due to the fact that
are specifically effective on the inflammatory
process
which characterises the
disease. Furthermore, there is strong evidence that
the addition of a LABA to a
daily ICS regimen improves asthma symptoms and lung
function, decreases
nocturnal asthma and the use of short-acting inhaled
β2-agonists, and reduces the number of exacerbations.
Thus, the preferred therapy for moderate persistent
asthma is regular treatment with a combination
of an ICS and a LABA
twice daily, and the primary therapy for severe
persistent asthma includes
ICS at higher doses plus a LABA.
In COPD, since the inflammatory process is not responsive
to steroids, the mainstays
of treatment are bronchodilators, including LABAs.
The benefits related to the addition of an ICS to a LABA have
been currently demonstrated only in patients with severe disease. |

